DISCUSSION: strategy for intrabony defects
The present case cohort assessed the clinical performance of a regenerative strategy developed to increase clinicians’ ability to optimize the outcomes of regenerative periodontal surgery. The overall rationale for the proposed clinical approach comes from the recognition that the different regenerative approaches reported in the literature frequently lead to unsatisfactory and rather unpredictable outcomes.

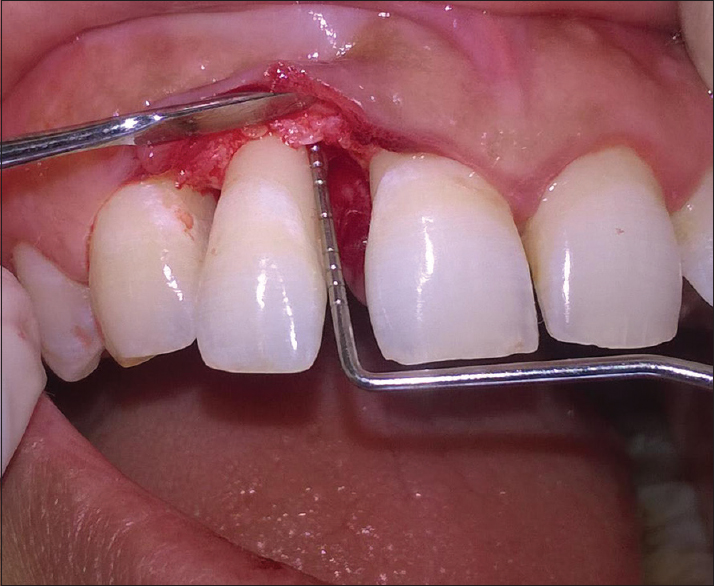
The proposed protocol (Figs. 1 and 2) is mainly based on different levels of scientific evidence and partly on the clinical experience of the authors. The published evidence allows us to clearly identify, and therefore to control, some of the factors that negatively influence the clinical outcomes of periodontal regeneration.
Patient-associated factors such as plaque control, residual periodontal infection, and smoking have been shown to have a consistent negative impact on both short- and long-term results. An ideal protocol for regenerative surgery should, therefore, include enough non-surgical periodontal therapy to minimize the impact of supragingival plaque and bacterial infection and smoking cessation protocols. Obtaining a high level of cooperation from the patient is also key: regenerative therapy requires a substantial contribution from the patient, in terms of compliance with a series of behavioral recommendations, modified oral hygiene methods, and topical and systemic medications.

Among the technical/surgical-associated factors, lack of primary closure of the interdental space and consequent bacterial contamination of the regenerating wound represents one of the most significant factors leading to compromised outcomes of regenerative surgery. An important element for improving regenerative outcomes is achieving and maintaining primary closure of the flaps in the critical interdental area. Modified flap designs allowing access to the defect area while preserving the interdental papilla have been shown to improve the ability of clinicians to obtain this goal, especially when used with a microsurgical approach. In the present study, the MPPT and the SPPF were used according to original indications: the MPPT to access wide interdental spaces (>2 mm) and the SPPF to access the narrower ones.
Selection of the regenerative strategy was based on some evidence and on some assumptions. Wide and non-supportive defects were treated with self-supporting membranes or with bioabsorbable barriers supported with a filler material. Our rationale was to avoid as much as possible the collapse of the barriers and of the overlying soft tissues into the coronal part of the defect. Such an occurrence is generally expected to reduce the space for regeneration and enhance the soft tissue recession. When defects were narrow and presented with a predominantly 2- or 3-wall morphology, a bioabsorbable barrier was used, assuming that the residual walls would prevent collapse of the barrier and soft tissues. In the 3-wall defects EMD was preferred based on evidence showing a positive response of 3-wall defects to EMD, which was also associated with a minimal impact of post-surgical complications.
Primary closure of the flaps was ensured by using a two-layer suturing technique. It consisted of a deep internal mattress suture aimed at coronal advancement of the flap and controlling flap tension, and of a more superficial internal mattress suture to close passively the interdental papilla.
A stringent post-surgical regimen was enforced to control bacterial contamination. A recent systematic review reports a significant PD reduction and an advantage in terms of CAL gains when a stringent postoperative plaque control regimen is followed.
The use of this decision-making protocol resulted in 6 ± 1.8 mm of CAL gain at 1 year in defects with an intrabony component of 6.6 ± 1.7 mm; CAL gain was 92.1% ± 12%. This indicates that a large part of the intrabony component of the defects was resolved. Using the Ellegaard and Löe criteria, resolution of the intrabony component of the defect was either satisfactory or complete in all treated cases. In particular, 40.5% of defects had attachment level gains equal or greater than the baseline depth of the intrabony component, while the defect with the worst response showed a 71.4 CAL%. Historical comparison with clinical experiments using bone grafting or GTR clearly indicates that the results of this trial are in the top percentiles in terms of CAL gains and defect resolution. To properly interpret these results, it is important to emphasize that several factors influence the clinical outcomes of periodontal regeneration. The case selection process excluded cases with sub-optimal patient-associated factors such as plaque control, residual bleeding on probing, or cigarette smoking.
Furthermore, the surgical procedures and regenerative materials used have been associated with a degree of sensitivity to the skills of the surgeon. In this respect, clinicians should not attribute the observed results to the choice of the regenerative strategy alone.
The increment in recession of the gingival margin between baseline and 1 year was only −0.1 ± 0.7 mm. This excellent result could be related to the interdental soft tissue preservation, the non-traumatic manipulation during surgery favored by the use of microsurgery, and the selection of the appropriate regenerative strategy which limited soft tissue collapse. The optimal clinical outcomes obtained with this approach are further underlined by the shallow residual probing depths of 2.7 ± 0.6 mm observed. These are relevant observations since one of the goals of regenerative treatment of intrabony defects is reduction of PD while causing minimal gingival recession.
Regarding primary closure of the flaps, it was technically possible to achieve complete primary closure in 100% of the treated interdental sites. Closure was maintained in 90% of cases for the entire healing period. Under these circumstances, it is reasonable to assume that wound healing occurred in a sealed environment with minimal levels of bacterial contamination and optimal stability of the wound. It is also evident that the ability to obtain and maintain primary closure allows optimal retention and biological activity of materials applied into the wound environment to differentially modulate the healing process.
This study was not intended to compare different regenerative approaches, but rather to give a rationale for the application of the different materials according to best clinical judgment. The results of the four groups of therapy, according to the regenerative material employed, show that each of the materials performed very well, with excellent clinical outcomes. This is especially evident in terms of percent clinical attachment gain. CAL% ranged from an average 95.4% ± 12.9% and 94.7% ± 13.4% with EMD and with titanium reinforced ePTFE membranes, respectively, to an average 88.9% ± 11.5% and 88.2% ± 9.6% obtained with bioabsorbable barriers alone and with bioabsorbable barriers supported by a bone replacement graft, respectively. Gingival recession observed and residual PD in each group were also minimal. The different morphology of the defects when a specific technology was applied, however, does not allow a comparative assessment in terms of performance since some of the morphologies are thought to represent greater clinical challenges than others. In conclusion, the use of the proposed regenerative strategy resulted in large amounts of clinical attachment level gains and minimal recessions at 1 year in all of the treated population and in each of the four treatment groups. It is, therefore, possible to suggest to clinicians wishing to optimize clinical outcomes of periodontal regeneration in intrabony defects to incorporate the operative strategies described in this study in their clinical decision making.
Related posts:
- Efektivitas Metode Motivasi pada Kebersihan Mulut Anak-anak
- Efektivitas Metode Motivasi pada Kebersihan Mulut Anak-anak
- Efektivitas Metode Motivasi pada Kebersihan Mulut Anak-anak
- Efektivitas Metode Motivasi terhadap Kebersihan Mulut Anak
- Efektivitas Metode Motivasi Anak-Anak pada Kebersihan Mulut Mereka
- Cara mudah akses posting baru kami
- Cara mudah mengikuti posting baru kami
- Cara mudah akses info gigi & mulut dari hp kamu
- Keefektifan Metode Motivasi terhadap Kebersihan Mulut Anak-anak
- Cara mudah ikuti posting baru pakai kamera hp
- Cara menyimpan sikat gigi agar terhindar dari bakteri
- Harga pasang kawat gigi di dokter gigi
- Kenali infeksi dekat implant gigi sedini mungkin
- Mengatasi bau mulut yang mengganggu
- Sudah Rajin Sikat Gigi Tapi Masih Bau Mulut?
- Cegah gigi berlubang dengan Fissure Sealants
- fissure-sealants
- GIGI GERAHAM BUNGSU / WISDOM TOOTH PERLUKAH UNTUK DICABUT?
- Veneer Gigi : alternative memutihkan tampilan gigi
- Usia ideal anak mulai sikat gigi sendiri
- Kapan anak dapat menyikat gigi sendiri?
- Mengatasi bau mulut yang mengganggu
- Anorexia nervosa & kesehatan gigi
- Erosi gigi
- Alasan kenapa gigi sensitif
- Cegah gigi berlubang dengan Fissure Sealants
- Cegah gigi berlubang dengan Fissure Sealants
- Cegah gigi berlubang dengan Fissure Sealants
- Cegah gigi berlubang dengan Fissure Sealants
- Implant gigi harga murah Rp 3 - 5 juta apa betulan ada?
- Crown gigi tahan berapa lama?
- Bagaimana cara agar gigi goyang cepat lepas dari gusi?
- Bagaimana cara agar gigi goyang cepat lepas dari gusi?
- Bagaimana cara agar gigi goyang cepat lepas dari gusi?
- Bagaimana cara agar gigi goyang cepat lepas dari gusi?
- menyambung gigi patah
- Berapa lama lubang bekas cabut gigi menutup?
- Cara menyimpan sikat gigi agar terhindar dari bakteri
- Harga pasang kawat gigi di dokter gigi
- Mengatasi bau mulut yang mengganggu
- Sudah Rajin Sikat Gigi Tapi Masih Bau Mulut?
- Cegah gigi berlubang dengan Fissure Sealants
- GIGI GERAHAM BUNGSU / WISDOM TOOTH PERLUKAH UNTUK DICABUT?
- Veneer Gigi : alternative pemutih gigi
- Kapan anak dapat menyikat gigi sendiri?
- 6 Cara menyimpan sikat gigi agar terhindar dari bakteri
- Anomalia Kelainan pada gigi
- Implan Gigi menurut pandangan Islam
- 10 Cara merawat gigi palsu dengan baik
- 3 Alasan mengapa harus menyikat gigi malam hari
- Benarkah Cabut Gigi Dapat Menyebabkan Kebutaan?
- Hisap jempol sebabkan tongos
- Flossing bermanfaat bagi kebersihan gigi
- Tentang kami
- Hubungi kami
- Visi
- Elemen visi
- Misi
- Nilai Inti
- Filosofi
- Struktur organisasi
- Tagline
- Sejarah
- Drg. Elisa
- Drg. Ika
- Drg. Irma
- Drg. Lita
- Drg. Mantili
- Drg. Margareth
- Drg. Wulan
- Drg. Novi
- Drg. Andreas Tjandra, FISID
- Tim Dokter
- Pasang implant gigi bagus & murah
- Pasang veneer gigi
- Fissure Sealants
- Layanan lain
- Memutihkan gigi
- Pasang behel
- Sertifikat
- Glosarium kedokteran gigi (Inggris - Indonesia)
- Definisi kedokteran gigi
- Sejarah implant gigi
- Drg. Angel
- Drg. Dita
- aswin - 2016-06-21 10:06:26
- Implan gigi
- Jadwal Praktik Klinik Pos Pengumben
- Jadwal Praktik "Doctor+Dentist" Palmerah
- Antisipasi Risiko Implan Gigi
- Implan gigi: solusi nyaman untuk gigi tanggal
- Bahan Implan Gigi
- Definisi osseointegrasi
- Prediktor kesuksesan implant gigi
- Keunggulan titanium untuk implant gigi
- Etimologi osseointegrasi
- Brånemark: bapak implant gigi modern
- Mekanisme osseointegrasi dalam implant gigi
- Prediktor kegagalan implant gigi
- Bahaya dan pencegahan karang gigi
- Gigi tanggal perlu diganti
- Diabetes mellitus dan implant gigi
- Tn. B*****
- Tn. F***** H. S******
- Ny. S****
- Ny. E***
- Tn. O**
- Nn. P**** D*** H***
- Tn. O** S** P**
- Tn. W*****
- Tn. A*********
- Tn. Y****
- Tn. M****** A******
- Tn. S****
- Tn. A***
- Nn. S*** H********
- Ny. N***
- Tn. I*******
- Tn. A**** B****
- Tn. S*******
- Tn. S*******
- Tn. P*****
- Ny. D*** C*********
- Tn. R***** A****
- Tn. K*** L*** M**
- Nn. N******
- Ny. V*****
- Tn. M******
- Tn. M. F***** I*****
- Ny. G***
- Kelebihan implant gigi
- Gigi sensitif dan penyebabnya
- Tambalan gigi amalgam (perak)
- Biaya & harga pasang + rawat implant gigi bagus & murah
- Tambalan gigi komposit
- Kelebihan / kekurangan tambalan gigi komposit
- Tambalan gigi emas
- Disclaimer
- Harga implant gigi relatif murah
- Pantangan implant gigi
- Akibat gigi ompong dibiarkan
- 7 alasan memilih implant gigi
- Implan gigi vs sistem bridge
- Implan gigi vs gigi palsu
- Pasang implant gigi tidak sakit
- Berapa lama pemasangan implant gigi?
- Impan gigi tahan berapa lama?
- Pengaruh rokok pada implant gigi
- Alergi pada bahan implant gigi
- Apa implant gigi bisa untuk lansia?
- Dokter gigi spesialis implant, adakah?
- Risiko bahaya perawatan implant gigi
- Tujuan utama implant gigi
- Siapa bisa memasang implant gigi?
- Tambalan GC Fuji IX
- Apakah implant gigi akibatkan kebutaan?
- Persiapan perawatan implant gigi
- Front office
- Instrumen perawatan gigi
- Perlu berapa implant untuk 3 gigi ompong?
- Kriteria/ syarat menerima implant gigi
- Kredit perawatan implant gigi
- Apa pemasangan implant gigi sakit?
- Apakah implant gigi bersifat permanen?
- Apa itu implant gigi?
- Terima kasih
- Tempat pasang implant gigi di Jakarta
- Apakah behel gigi bisa dibayar dicicil?
- Apakah implant gigi total berbahaya?
- Apakah usia 50 tahun bisa implant gigi?
- Berapa maksimal umur pemakaian perawatan behel?
- Bagaimana cara menghilangkan iritasi akibat kawat gigi?
- Apakah implant gigi aman?
- Apakah gigi ompong 3 bisa diimplant?
- Kenapa gigi implant saya bau?
- Solusi gigi berlubang yang sudah tidak bisa ditambal
- Dapatkah Behel merapatkan gigi?
- Apa yang akan terjadi setelah pemasangan implant gigi selesai?
- Bagaimana jika tubuh menolak implant gigi?
- Berapa lama waktu menunggu implant gigi jadi?
- Berapa harga gigi tanam permanen?
- Alamat doctor+dentist, klinik gigi & implant gigi Jakarta
- Apa larangan setelah pasang gigi implant?
- Harga gigi palsu depan
- Apa tanda dan gejala kanker mulut?
- Apakah veneer bersifat permanen?
- Apakah gigi yang patah bisa disambung lagi?
- Drg. Andreas Tjandra dalam
- Apakah gigi patah bisa diveneer?
- Cara memutihkan gigi
- Kenapa kok gigi artis bisa putih banget?
- Berapa biaya pemasangan implant gigi saja?
- Cara merawat veneer gigi
- Pasang veneer pada gigi keropos
- Makanan yang dilarang bagi pemakai/ pengguna behel
- Implan gigi: Before & After
- Tambalan gigi inlay/ onlay
- Akibat gigi ompong
- Rahasia awet muda dengan implant gigi
- Beda gigi palsu permanen & implant gigi/ tanam gigi
- Reza Pahlevi
- Periodontitis: Pencegahan & dampak
- Tanda, gejala, dan pemeriksaan periodontitis
- Gigi implant goyang
- 11 cara merawat gigi palsu
- Harga implant gigi depan
- Persiapan pasang implant gigi
- Cara memilih warna terbaik behel
- Mengatasi bau mulut pagi hari
- Apa penyebab infeksi pada gigi yang sudah diimplant?
- Jenis Implan Gigi Paling Umum
- Mulai berapakah harga implant gigi termurah?
- 8 Bahaya & Efek Samping Implan Gigi & Antisipasinya
- Implan gigi cocoknya untuk siapa?
- Betulkah kunyit memutihkan gigi?
- Benarkah minyak zaitun bisa memutihkan gigi?
- Apa cara paling mudah memutihkan gigi kuning karena nikotin?
- Kontraindikasi Implan Gigi
- Jenis dan Klasifikasi Implan Gigi
- Kelemahan implant gigi
- Implan gigi sehari jadi
- Operasi pasang implant gigi
- Kenapa gigi bisa kuning?
- Meninggal dunia karena implant gigi????
- Indikasi Implan Gigi
- Gigi implant & makanan keras
- Jumlah implant gigi maksimal
- Penyebab infeksi pada implant gigi beserta antisipasi
- Cara memilih dokter gigi implant
- Bone graft & implant gigi pada rahang menciut
- Selisih waktu cabut gigi & implant gigi
- Makan lunak setelah implant gigi
- Cara dapat implant gigi gratis
- Berapa tingkat kegagalan implant gigi?
- Proses oseointegrasi pada implant gigi
- Perbaikan tulang di daerah implant
- Fibrointegrasi VS Oseointegrasi
- Implan gigi mini
- Anestesi lokal implant gigi
- Antibiotika sebelum implant gigi
- Cara dapat implant gigi murah banget
- Saran setelah implant gigi
- Segel biologis implant gigi
- Penjangkaran implant secara mekanik & bioaktif
- Zirkonia: Implan bebas logam
- Klasifikasi kepadatan tulang
- Asam merusak implant gigi?
- Apa implant titanium bisa berkarat?
- Tahap oseointegrasi pada implant gigi
- Efek kortikosteroid pada implant gigi
- Risiko implant gigi yang terlalu murah
- Kegagalan implant gigi
- Faktor yang memengaruhi oseointegrasi
- Implan sistem Branemark
- Definisi peri-implantitis
- Penyebab peri-implantitis
- Bahan implant gigi
- Implan gigi aman
- Benarkah implant zirkonia lebih baik daripada titanium?
- Kriteria sukses implant gigi
- Indeks estetika mahkota implant gigi
- Antisipasi faktor eksogen kegagalan implant awal
- Mekanisme oseointegrasi pada implant gigi
- Pemenang penghargaan EAO bidang implant gigi
- MED - teknologi stimulator implant gigi
- Penyembuhan luka operasi menggunakan makanan
- Obat depresi berkaitan dengan kegagalan implant
- Respon jaringan tulang pada implant gigi
- Prinsip Pedoman Umum Gerard Byrne
- Reaksi tubuh pada benda asing
- Evaluasi kepuasan pasien implant gigi
- Apa gigi implant bisa berlubang?
- Penentu penjangkaran implant gigi
- Analisis frekuensi resonansi (RFA) & stabilitas implant
- Tes torsi terbalik (Reverse torque test)
- Analisis CTR (Cutting Torque Resistance)
- Analisis radiografi
- Analisis RFA (Resonance Frequency Analysis)
- Implan nanotube temuan Dr. Cortino Sukotjo
- Osteoporosis dan implant gigi
- Implan gigi vs terapi radiasi
- Stabilitas implant gigi
- Skala kesehatan implant James - Misch
- Garansi implant gigi
- Implan gigi harga murah Rp 3 - 5 juta. Betulkah ada?
- Implan gigi: Mitos vs Kenyataan
- Implan gigi pada masa hamil
- Alergi titanium
- Jika implant gigi gagal, apa tetap bayar?
- 7 Fakta menarik tentang implant gigi
- Andai implant gagal, apa yang akan terjadi?
- Apa pentingnya stabilitas implant?
- Cara mencegah ompong
- 4 Musuh Implan Gigi
- Gerakan implant gigi
- Propriosepsi: Pengertian, definisi, dan teori
- Alternatif untuk implant gigi
- Radiografi untuk implant gigi
- Rekam medik implant gigi
- Malpraktik implant, mungkinkah terjadi?
- Bagaimana cara mengantisipasi risiko implant gigi?
- Tingkat kesuksesan implant 20 tahun setelah pemasangan
- Kontak Implan-Tulang
- Permukaan implant gigi
- Pasien bisa mendeteksi dini masalah implant
- Robot implant gigi masa datang
- Kekasaran permukaan implant gigi
- Terapi HBO dan implant gigi
- Perlakuan permukaan implant gigi
- Faktor penyusutan tulang tahap akhir
- Apa semua orang yang ompong bisa dirawat implant?
- 7 Poin perlu diketahui sebelum implant gigi
- Permintaan implant gigi
- Dampak psikologis ompong
- 13 Faktor terkait ompong
- 10 Selebritis Dengan Perawatan gigi kosmetik
- Detektor logam bandara & implant gigi
- 7 Alasan tak perlu cemas dengan implant gigi
- Panas bisa menggagalkan implant gigi
- 7 Alasan melepas implant gigi
- Cara melepas implant gigi
- Solusi menurunkan panas tulang rahang
- Makanan - minuman panas & implant titanium
- Apa implant titanium sekuat dalam film X-men?
- Perawatan saluran akar atau implant gigi?
- Pemandu bedah implant gigi
- 5 Ramalan dunia implant gigi masa datang
- Implan gigi dalam peradaban kuno
- Bukti perawatan gigi pada jaman batu
- Bor gigi jaman batu muda dari Mehrgarh
- Pemeliharaan implant gigi
- Kelemahan implant gigi
- Tips meredakan pendarahan pasca-operasi implant
- Hubungan rokok dan permasalahan gigi
- Tambalan gigi era purbakala
- Hepatitis C & implant gigi
- Stabilitas prostetik-implant: sekrup atau semen
- Reoseointegrasi untuk menangani implant gagal
- Peran darah untuk kesuksesan implant gigi
- 9 Faktor pendukung oseointegrasi
- 7 Faktor penghambat oseointegrasi
- Osteoinduksi
- Osteokonduksi
- Peran osteoblas dalam implant gigi
- Materi bone graft
- Autograft (autogenous bone graft)
- Allograft (Allogenic bone graft)
- Sel induk mesenkim
- BMP (Bone Morphogenetic Protein)
- TGF-β (Transforming Growth Factor-β)
- PDGF (Platelet-derived growth factor)
- FGF (Fibroblast growth factor)
- IGF atau ILGF (Insulin-like growth factors)
- Osteoblas
- RANKL
- RANKL: struktur, fungsi, & peran
- Osteoklas, sel pemangsa tulang
- Ekspresi gen dalam osteoblas
- L-PRF mempercepat penyembuhan
- Hemostasis
- FGF-2 dalam perawatan implant
- Osteosit
- Osteogenesis
- Hemostasis tulang
- Sejarah sikat gigi
- Pemodelan ulang tulang (bone remodelling)
- Resorpsi tulang
- Sel pelaku pemodelan ulang tulang
- Sel sistem kekebalan tubuh
- Sel T
- Sel B, sel tukang sapu
- Megakaryosit
- Osteomak (Osteo makrofag)
- Faktor yang memengaruhi pemodelan ulang tulang
- Mineralisasi
- Pirofosfat
- Pemodelan tulang
- Hidroksiapatit
- Sakit gigi dan kesehatan jiwa
- Inflamasi tulang
- Fibroblas
- Jaringan tulang
- Odontoblas
- Diferensiasi sel induk pulpa
- Sel induk pulpa gigi (DPSC)
- Matriks ekstraseluler
- Diferensiasi
- Runx2
- Osterix
- Bakteri dalam mulut
- Actinomyces
- Cbfa1
- Osteokalsin
- Osteopontin (OPN)
- Struktur osteopontin
- Fungsi dan peran osteopontin
- Osteopontin dan mineralisasi
- Osteopontin (OPN) dan sistem kekebalan tubuh
- Mikroba dan implant gigi
- Biomaterial
- Streptococcus mutans
- Treponema denticola
- Porphyromonas gingivalis
- Virulensi Porphyromonas gingivalis
- Tannerella forsythia
- Probiotik
- Kolagen
- Homeostasis
- Sejarah kuno kedokteran gigi
- Jaringan ikat
- TNF-α
- Osteoprotegerin (OPG)
- RANK
- Pierre Fauchard - Bapak Kedokteran Gigi Modern
- Dr. John M. Harris - Pendiri Sekolah Kedokteran Gigi Pertama
- Emeline Roberts Jones - Perintis sarjana dokter gigi perempuan
- Amalia Assur - Dokter gigi perempuan pertama
- 10 Ciri dokter gigi yang bagus
- C. Edmund Kells - Martir rontgen gigi
- Milton Waldo Hanchett - Pencipta kursi gigi
- Tambalan bebas air raksa
- Gigi patah pada bagian enamel-dentin
- Gigi gumpil (fraktur enamel)
- Fraktur enamel - dentin - pulpa
- Patah rahang
- Infraksi enamel (Gigi retak)
- Erosi gigi
- Enamel
- Dentin
- Efek minuman beralkohol pada gigi
- Meredakan ngilu pada gigi sensitif
- Hipoplasia enamel & gigi sensitif
- Amelogenesis imperfekta & gigi sensitif
- Dentinogenesis imperfecta
- Sindrom TDO dan gigi sensitif
- Merawat dentinogenesis imperfecta
- Evolusi kursi gigi (abad 18-19 Masehi)
- Fobia gigi (dental phobia)
- Anorexia nervosa & kesehatan gigi
- Evolusi kursi gigi abad 20-21 Masehi
- Bulimia nervosa & kesehatan gigi
- Dr. Francis Rynd - penemu jarum suntik
- Mulut kering (xerostomia)
- Tips mencegah gigi berlubang
- William Thomas Green Morton - anestesia publik pertama
- Sakit gigi
- Mengatasi kecemasan gigi (dental anxiety)
- Kegunaan berkumur air garam
- Tren gigi drakula dari Jepang (yaeba)
- Print 3 dimensi untuk membuat gigi palsu
- Wisata perawatan gigi
- Perawatan enameloplasty
- Penemuan sinar X (sinar röntgen)
- Benarkah minyak kelapa mengobati gigi berlubang?
- Gigi kelinci
- Gigi gingsul (gigi bertumpuk)
- Apa beda implant gigi dan tanam gigi?
- Xenograft (Xenogenic bone graft)
- Alloplastic bone graft (Alloplast)
- Kelainan dentin
- Dentine dysplasia
- Kontroversi "abadi" penggunaan amalgam
- Bisakah ozon mencegah gigi berlubang?
- Fondasi implant gigi
- Kenapa ada perawatan implant murah dan mahal?
- Bone graft : teknologi abad 17 Masehi
- Pelindung gigi pasca implant apakah perlu?
- Gigi bau padahal sudah sikat gigi
- Kenali infeksi implant sedini mungkin
- Osteomyelitis
- Kenapa rokok menyebabkan mulut bau tidak enak?
- Kenapa mulut saya terasa pahit/ asin?
- Prostaglandin dan obat nonsteroid antiinflamasi
- Biofilm
- Berapa banyak organisme mikro dalam mulut manusia?
- Karang gigi & pencegahannya
- Inflamasi tulang (osteitis)
- Penyembuhan luka bedah di sekitar implant gigi
- Oseointegrasi
- Tulang anyam (woven bone)
- Tulang lamelar
- Biokompatibilitas
- Penilaian klinis oseointegrasi
- Penentu sukses oseointegrasi implant gigi (1)
- Penentu sukses oseointegrasi implant gigi (2)
- Penentu sukses oseointegrasi implant gigi (3)
- Tes biokompatibilitas materi implant
- Sitokin mempercepat penyembuhan pasca implant
- Bahaya nikotin
- Penyakit periodontal (penyakit gusi)
- Neutrofil
- Basofil
- Bahan biomaterial (1)
- Bahan biomaterial (2)
- Bahan biomaterial (3)
- Cek gigi Anda sebelum hamil
- Sakit gigi saat naik pesawat terbang
- Bahaya karang gigi
- Faktor risiko dan pencegahan penyakit periodontal
- Penyebab penyakit periodontal (gusi)
- Cara mencegah gusi berdarah
- 12 penyebab gusi berdarah
- Plak
- Tulang alveolar
- Tulang kortikal
- Gigi berlubang (kavitas)
- Restorasi mahkota dowel (1)
- Restorasi mahkota dowel (2)
- Restorasi mahkota dowel (3)
- Restorasi mahkota dowel (4)
- Mengatasi 9 masalah gigi yang paling umum
- Infeksi akar gigi
- Tanda & gejala infeksi gigi
- Pulpa gigi
- Apa penyebab lidah pigmentasi?
- Apa gigi berlubang bisa menular ke gigi lain?
- Kenapa gigi perokok kuning?
- 6 tips menghindari karang gigi
- Beberapa bagian gigi menghitam, kenapa?
- Apa sisa akar dalam gusi perlu dicabut? Apa bahaya jika tidak dicabut?
- Cara memilih sikat gigi yang baik
- Cara memilih pasta gigi yang bagus
- Merencanakan perawatan implant di daerah estetis (1)
- Merencanakan perawatan implant di daerah estetis (2)
- Seleksi dan garis senyum pasien
- Posisi gigi
- Posisi akar gigi di sebelah lokasi implant
- Biotipe periodontium dan bentuk gigi
- Anatomi tulang daerah implant
- Struktur anatomi penentu pasca implant
- Posisi implant
- Penempatan implant pada arah apiko-koronal (1)
- Penempatan implant pada arah apiko-koronal (2)
- Penempatan implant pada arah mesio-distal
- Penempatan implant pada arah fasio-lingual
- Pertimbangan penanaman implant gigi multipel (1)
- Pertimbangan penanaman implant gigi multipel (2)
- Pertimbangan penanaman implant gigi multipel (3)
- Implan gigi sebagai solusi final
- Glossitis migran jinak (lidah geografis)
- Lidah berbulu hitam
- Ulkus lidah kronis / sariawan kronis
- Cedera akibat gigi palsu
- Luka bakar dalam mulut akibat tersengat listrik
- Luka bakar termal pada mulut
- Luka bakar di mulut karena makanan oven
- Mukositis karena Radiasi
- Cedera oral sebagai dampak dari terapi radiasi
- Definisi kedokteran mulut
- Kedokteran gigi dan mulut dalam rumah sakit
- Hubungan penyakit kulit dan penyakit mulut
- Remineralisasi gigi
- Triklosan
- Fluorida
- Infeksi Virus Herpes
- Demineralisasi gigi
- Tanam implant gigi depan rahang atas
- Rencana pemasangan implant gigi depan rahang atas (1)
- Rencana pemasangan implant gigi depan rahang atas (2)
- Pelaksanaan pemasangan implant gigi depan rahang atas
- Rehabilitasi prostetik implant gigi depan rahang atas
- Rekayasa Jaringan Lunak dalam Kedokteran Gigi
- Alograft Aselular
- Derivasi matriks enamel (1)
- Derivasi matriks enamel (2)
- Derivasi matriks enamel (3)
- Kenapa gusi saya berwarna hitam?
- Implan berdiameter kecil
- Panas memengaruhi kesuksesan implant gigi
- Infeksi Virus Herpes Simplex Primer (1)
- Infeksi Virus Herpes Simplex Primer (2)
- Manifestasi Klinis Herpes Simplex Mulut Primer
- Diagnosis Laboratorium Herpes Simplex Oral
- Perawatan Herpes Simplex Oral Primer (Acyclovir)
- Herpangina
- Penyakit kaki, tangan, dan mulut (PKTM)
- Infeksi Virus Varicella Zoster (VZV)
- Temuan umum manifestasi klinis virus Varicella Zoster (VZV)
- Temuan oral manifestasi klinis virus Varicella Zoster (VZV)
- Perawatan infeksi virus Varicella Zoster (VZV)
- Eritema multiformis
- Temuan umum manifestasi klinis Eritema Multiformis
- Temuan oral manifestasi klinis Eritema Multiformis
- Perawatan Eritema Multiformis
- Stomatitis alergi
- Manifestasi klinis stomatitis alergi
- Pertimbangan neurovaskular dalam implant gigi: Pengantar (1)
- Pertimbangan neurovaskular dalam implant gigi: Pengantar (2)
- Anatomi saraf rahang bawah (1)
- Tanam implant gigi
- Waktu tanam dan penyembuhan implant gigi
- Biokompatibilitas biomateri implant gigi
- Titanium & Vanadium pas untuk implant gigi
- Apakah gigi krowok bisa menular ke gigi yang lain?
- Epidemiologi kanker mulut
- Berapa umur untuk memasang gigi implant?
- Apa makanan yang aman dimakan setelah implant gigi?
- Interaksi jaringan dengan implant gigi
- Pembentukan paduan implant gigi dengan tulang rahang
- Apakah implant gigi aman?
- 10 kesalahan dalam menyikat gigi
- Respon tubuh terhadap biomateri implant gigi
- Penguncian implant pada tulang
- Bagaimana baiknya setelah operasi implant gigi?
- Kenapa implant tidak boleh bergerak?
- Prosedur implant pembebanan langsung
- Berapa lama proses implant gigi?
- Bagaimana mencegah penyakit gusi?
- Bisakah gigi berlubang sembuh sendiri & menutup sendiri?
- Benarkah minyak kelapa bisa menyembuhkan gigi berlubang?
- Apakah asam fitat berbahaya buat gigi?
- Ameloblastin, pembentukan akar gigi dan perkembangannya
- Sekilas tentang peran ameloblastin dalam pembentukan akar
- Peran ameloblastin dalam pembentukan enamel gigi
- Injeksi siRNA ameloblastin menyingkap pembentukan akar gigi
- Ameloblastoma dan Kista Dentigerus Terkait Impaksi Gigi (3)
- Ameloblastoma dan Kista Dentigerus Terkait Impaksi Gigi (4)
- Ameloblastoma dan Kista Dentigerus Terkait Impaksi Gigi (1)
- Ameloblastoma dan Kista Dentigerus Terkait Impaksi Gigi (2)
- Kesuksesan implant perlu lapisan titanium oksida (1)
- Kesuksesan implant perlu lapisan oksida titanium (2)
- Interaksi sel dengan permukaan biomateri (1)
- Interaksi sel dengan permukaan biomateri (2)
- Interaksi sel dengan permukaan biomateri (3)
- Interaksi sel dengan permukaan biomateri (4)
- Implan gigi harga 3 juta, ada kah?
- Mungkinkah implant gigi bisa lepas?
- Apakah minyak kelapa bisa menutup gigi busuk?
- Setelah gigi rusak dicabut, kapan bisa pasang implant gigi?
- Perawatan bone graft berapa lama?
- Apakah cabut gigi bisa menyebabkan rabun?
- Apa bisa gigi implant untuk gusi yang sudah menipis?
- Apa efek miras pada gigi & mulut?
- Berapa lama proses implant gigi yang paling cepat?
- Produk implant gigi yang aman itu seperti apa?
- Tipe implant gigi (1)
- Tipe implant gigi (2)
- Risiko dan Penanganan Komplikasi Implan Gigi
- Rehabilitasi mulut lengkap dengan perlekatan ekstrakoronal (1)
- Rehabilitasi mulut lengkap dengan perlekatan ekstrakoronal (2)
- Rehabilitasi mulut lengkap dengan perlekatan ekstrakoronal (3)
- Rehabilitasi mulut lengkap dengan perlekatan ekstrakoronal (4)
- Kekasaran permukaan implant faktor sukses implant gigi (1)
- Kekasaran permukaan implant faktor sukses implant gigi (2)
- Kekasaran permukaan implant faktor sukses implant gigi (3)
- Kekasaran permukaan implant faktor sukses implant gigi (4)
- Implan gigi emas, mungkinkah?
- Kekasaran permukaan implant faktor sukses implant gigi (5)
- Merawat gigi berlubang tanpa bor dan penambalan, mungkinkah?
- Bagaimana cara merawat gigi yang baik?
- Berapa kisaran harga implant gigi murah di Jakarta?
- Perawatan implant gigi perlu tindak lanjut
- Penilaian kesehatan implant (3)
- Indeks plak untuk implant gigi
- Pasien sakit ginjal menerima implant gigi, bisakah?
- Cara mengobati gusi bengkak bagaimana?
- Penilaian kesehatan implant (1)
- Penilaian kesehatan implant (2)
- Diagnosis & penanganan kesehatan implant gigi (1)
- Penilaian kesehatan implant (4)
- Diagnosis & penanganan kesehatan implant gigi (2)
- Pengaruh permukaan implant pada stabilitas primer (1)
- Pengangkatan geraham bungsu (wisdom tooth)
- Pengaruh permukaan implant pada stabilitas primer (2)
- Keterbasahan implant
- Pengaruh tulang pada kesuksesan implant gigi
- Apakah rahang bawah patah bisa tersambung lagi?
- Apakah tulang rahang tipis bisa implant?
- Pertolongan pertama pada patah rahang
- Dampak cengkeh pada gigi & plak
- Apakah orang pakai gigi palsu bisa masuk kerja di perusahaan?
- Pengaruh permukaan implant pada pemaduan implant dengan tulang (1)
- Pengaruh permukaan implant pada pemaduan implant dengan tulang (2)
- Perlakuan permukaan implant (1)
- Perlakuan permukaan implant (2)
- Perlakuan permukaan implant (3)
- Implan laser & plasma (1)
- Implan laser & plasma (2)
- Permukaan implant dengan perlakuan etsa asam
- Semburan partikel pada permukaan implant gigi
- Apa kelebihan gigi emas?
- Kenapa gula merusak gigi?
- Gigi sakit padahal sudah ditambal, kenapa?
- Permukaan implant dengan perlakuan fluorida (1)
- Permukaan implant dengan perlakuan fluorida (2)
- Implan dengan kekasaran nano
- Eksploitasi mulut oleh bakteri / mikroba
- Kontrol bakteri dalam mulut
- Metode pemberian antibakteri dalam mulut pasien
- Menyingkap biofilm gigi (1)
- Menyingkap biofilm gigi (2)
- Pedoman kebersihan mulut
- Bahaya! Gigi berlubang bisa bikin buta!
- Abses periapikal
- Gejala/ tanda abses gigi
- Abses: apa, kenapa, & gejala
- Abses periodontal
- Pengertian abses
- EYD bidang kedokteran gigi implant
- Infeksi odontogenik: selayang pandang
- Mikrobiologi infeksi odontogenik
- Gingivitis itu apa?
- Bakteri dalam infeksi odontogenik
- Tahap-tahap infeksi odontogenik
- Infeksi odontogenik menyebar ke jaringan rentan
- Infeksi odontogenik memakan tulang sekitar
- Riwayat lengkap infeksi odontogenik (1)
- Riwayat lengkap infeksi odontogenik (2)
- Pemeriksaan fisik infeksi odontogenik (1)
- Pemeriksaan fisik infeksi odontogenik (2)
- Pemeriksaan fisik infeksi odontogenik (3)
- Pemeriksaan fisik infeksi odontogenik (4)
- Pantangan setelah membersihkan karang gigi
- Apakah karang gigi menyebabkan bau mulut?
- Kondisi medis pengganggu pertahanan tubuh pasien
- Gangguan kekebalan tubuh
- Respon imun & faktor genetik pelawan infeksi
- Penghalang infeksi natural
- Menentukan rujukan pasien infeksi odontogenik (1)
- Menentukan rujukan pasien infeksi odontogenik (2)
- Menentukan rujukan pasien infeksi odontogenik (3)
- Abses dental
- Bahan restorasi gigi dengan partikel nano
- Partikel nano yang paling menjanjikan
- Bahan restorasi gigi dengan properti anti-mikroba (1)
- Bahan restorasi gigi dengan properti anti-mikroba (2)
- Kadar anti-mikroba yang efektif dan aman
- Anti-mikroba pada tambalan sementara
- Keseimbangan dalam bahan restorasi
- Betulkah emas bisa mematikan bakteri?
- Crown gigi tahan berapa lama?
- Menyingkap biofilm gigi (3)
- Benarkah air liur itu steril / bersih?
- Nama dan jumlah tulang dan sendi atau ligamen manusia
- Benarkah permen membuat gigi berlubang?
- Apa beda implant gigi dengan gigi palsu permanen?
- Granuloma periapikal (periodontitis apikal kronis)
- Saraf alveolar inferior penting dalam perawatan implant
- Reposisi saraf alveolar inferior dalam operasi implant
- Anatomi saraf mandibular (1)
- Anatomi saraf mandibular (2)
- Anatomi saraf mandibular (3)
- Anatomi saraf mandibular (4)
- Anatomi saraf mandibular (5)
- Anatomi saraf mandibular (6)
- Anatomi saraf mandibular (7)
- Anatomi saraf mandibular (8)
- Anatomi saraf mandibular (9)
- Morfologi saraf
- Cedera saraf neuropraxia
- Cedera saraf Axonotmesis
- Implan gigi mempertahankan kesehatan gigi di sekitarnya
- Garis besar prosedur implant
- Neurotmesis (saraf putus)
- Penanaman implant dengan teknik lateralisasi saraf alveolar inferior
- Implan generasi kedua terbukti lebih cepat dan lebih kuat
- Teknologi mikro dan nano dalam implantologi
- Kekasaran permukaan implant titanium
- Permukaan implant generasi pertama
- Sandblast (semburan partikel)
- Perlakuan etsa asam
- Implan permukaan SLA
- Permukaan anodisi
- Permukaan dilaser
- Lapisan kalsium fosfat pada implant titanium
- Metode persiapan lapisan CaP pada implant
- Karakteristik metode persiapan CaP
- Permukaan disemprot plasma
- Deposisi sputter
- Presipitasi biomimetik
- Lapisan kaca bioaktif
- Faktor-faktor dalam diagnosis dan perencanaan perawatan
- Diabetes & kesehatan mulut
- Penyakit jantung dan kesehatan mulut
- Seberapa sering kontrol ke dokter gigi?
- Respon jaringan terhadap modifikasi permukaan implant (1)
- Respon jaringan terhadap modifikasi permukaan implant (2)
- Mulut kering (xerostomia) dan hal-hal terkait
- Respon jaringan terhadap modifikasi permukaan implant (3)
- Respon jaringan terhadap modifikasi permukaan implant (4)
- Respon jaringan terhadap modifikasi permukaan implant (5)
- Respon jaringan terhadap modifikasi permukaan implant (6)
- Ultrastruktural antarmuka implant - tulang
- Metode preparasi sampel TEM
- Analisis antarmuka permukaan implant (1)
- Analisis antarmuka permukaan implant (2)
- Pengujian implant sebelum aplikasi
- Organisasi standar implant internasional
- Bahan dan metode evaluasi implant (1)
- Bahan dan metode evaluasi implant (2)
- Anomali dentofasial / maloklusi
- Pencegahan dan perawatan anomali dentofasial
- Fluorosis gigi
- Lantaran & gejala Fluorosis
- Penanganan dan pencegahan fluorosis
- Paleopatologi gigi dan mulut
- Kegunaan gigi di bidang lain
- Gigi berlubang ada sejak jutaan tahun lalu
- Bagaimana ceritanya manusia kena sakit gigi?
- Karbohidrat sumber karies sepanjang masa
- Penyebaran penyakit gigi berlubang
- Apa yang dilakukan peradaban kuno untuk menangani sakit gigi?
- Kuantifikasi beban inflamasi area permukaan akar (1)
- Kuantifikasi beban inflamasi area permukaan akar (2)
- Kuantifikasi beban inflamasi area permukaan akar (3)
- Kuantifikasi beban inflamasi area permukaan akar (4)
- Kuantifikasi beban inflamasi area permukaan akar (5)
- Kuantifikasi beban inflamasi area permukaan akar (6)
- Kuantifikasi beban inflamasi area permukaan akar (7)
- Kuantifikasi beban inflamasi area permukaan akar (8)
- Kuantifikasi beban inflamasi area permukaan akar (9)
- Sel induk folikel gigi dan rekayasa jaringan (1)
- Sel induk folikel gigi dan rekayasa jaringan (2)
- Sel induk mesenkim dalam folikel dental
- Sumber sel induk folikel dental
- Kapasitas diferensiasi sel induk folikel gigi
- Potensi proliferasi & diferensiasi sel induk folikel gigi
- Dari proliferasi ke diferensiasi sel induk folikel gigi
- Lokasi sel induk folikel gigi
- Kemampuan sel folikel gigi membentuk jaringan tulang
- Sel induk folikel gigi mendukung pembentukan tulang baru
- Rekayasa jaringan periodontal
- Sumber sel alternatif terapi regenerasi periodontal
- Transplantasi sel induk terbukti menghasilkan struktur akar gigi
- Tujuan penjahitan luka bedah gigi
- Dasar menjahit luka bedah (1)
- Bagaimana cara agar gigi goyang cepat lepas dari gusi?
- Prinsip-Prinsip Pedoman Umum Menjahit Luka Bedah
- Benang bedah
- Degradasi jahitan bedah gigi
- Teknik jahitan terputus sederhana (1)
- Teknik jahitan terputus sederhana (2)
- Setelah membersihkan karang gigi, apa yang perlu dilakukan?
- Apa efek samping membersihkan karang gigi?
- Apa dampak negatif membersihkan karang gigi?
- Membersihkan karang gigi bikin ngilu? Solusi apa?
- Pengalaman membersihkan karang gigi
- Betulkah membersihkan karang gigi bisa bikin gigi goyang?
- Apa crown gigi punya efek samping/ risiko?
- Apa guna perawatan crown gigi?
- Betulkah crown pada gigi bisa bertahan selamanya?
- Simple interrupted suture (Jahitan terputus sederhana)
- Bagaimana cara mengatasi gusi hitam?
- Benarkah minyak cengkeh bisa memerahkan gusi hitam?
- Teknik jahitan kontinyu sederhana
- Gusi saya hitam padahal tidak merokok, kenapa ya?
- Apa karang gigi bisa lepas sendiri?
- Apa efek samping terlalu sering membersihkan karang gigi?
- Cara mengatasi ngilu setelah pembersihan karang gigi?
- Bagaimana cara mengetahui sisa akar gigi yang tertinggal setelah dicabut?
- Bagaimana cara mengatasi sisa akar gigi yang tertinggal setelah cabut gigi?
- Gigi ompong di usia muda
- 13 faktor pemicu air liur jadi terasa asin
- Tusuk gigi teknologi purbakala
- Persiapan mulut untuk gigi tiruan parsial lepasan
- Pengertian cairan saliva dan sekresi protein
- Titanium Plasma Spray (TPS) / Semprotan Plasma Titanium
- Dukungan untuk Titanium Plasma Spray (TPS)
- Ekspansi Nobel Biocare : CAD/ CAM yang menawarkan fleksibilitas dan konektivitas
- Membuat gusi hitam jadi merah muda (pink)
- Abses palatal pada pasien pediatri
- Berapa biaya implant gigi jika banyak gigi yang copot?
- Apa itu pericoronitis?
- Pericoronitis: diagnosis dan perawatan
- Anatomi Periodontium
- Sulkus gingiva dan gingiva terlekat
- Gingiva interdental
- Epitelium gingiva
- Desmosom & interkoneksi keratinosit
- Fungsi utama epitel gingiva
- Sel-sel Langerhans
- Pasang implant gigi itu sakit apa tidak?
- Gigi palsu permanen apa betul ada?
- Benarkah implant gigi gampang copot?
- Benarkah semua dokter bisa memasang implant gigi?
- Membersihkan gigi implant ribet nggak?
- Betulkah implant gigi mematikan?
- Berapa lama lubang bekas cabut gigi menutup?
- Istilah cabut gigi dalam kedokteran gigi
- Implan gigi depan atas
- Bagaimana tingkat komplikasi perawatan implant gigi?
- Apa beda gigi implant dan gigi palsu permanen?
- Implant gigi itu apa?
- Tingkat kejadian gigi ompong
- Apa beda gigi implant dan gigi palsu?
- Kenapa gigi implant bisa populer?
- Apakah implant gigi sakit?
- Apa tanam implant gigi perlu bius?
- Implant gigi meningkatkan hubungan sex
- Apa gigi implant dipasang pakai lem perekat gigi palsu permanen?
- 2 gigi geraham saya sudah dicabut. Apa bisa pasang 2 sekaligus?
- Apa crown gigi implant seawet implant gigi?
- Kenapa orang pasang implant gigi?
- Apakah tubuh manusia bisa menerima benda asing implant gigi?
- Implant gigi expandable pendek
- Implant gigi expandable & pendek untuk gusi yang sudah susut
- Indikasi dan kontra indikasi oral hygiene
- Apa efek pasang gigi model gigi tanam tub?
- Berapa harga implant gigi 2018?
- Apa desain implant memengaruhi stabilitas primer implant?
- Bagaimana jika dokter membor terlalu dalam saat menyiapkan lubang untuk implant?
- Gigi palsu permanen tahan berapa lama?
- Klinik dental implant Jakarta ada di mana?
- Berapa lama pasang gigi palsu tanam setelah cabut gigi?
- Makanan yang tidak boleh dimakan oleh orang yang memasang implant gigi apa saja?
- Berapa harga gigi implant semua?
- Betulkah gigi implant membuat bau mulut?
- Efek rokok pada implant gigi
- Berapa harga termurah pasang implant gigi?
- Dampak positif implant gigi apa saja?
- Mengganti geraham bawah dengan implant gigi
- Implant gigi terutama untuk mengatasi ompong
- Gigi implant - gigi palsu paling mirip gigi asli
- Bagaimana jika ompong geraham kedua tidak diganti?
- Perawatan implant gigi tuntas sehari, mungkinkah?
- Aneka prosedur implant gigi
- Implant gigi apa selalu lebih baik daripada gigi palsu biasa?
- PENILAIAN PENGARUH TERAPI FOTODINAMIK PADA PENGOBATAN PERIODONTITIS SEDANG SAMPAI BERAT: STUDI PERCOBAAN KLINIS ACAK
- Suntik gigi
- Proses penyuntikan gigi
- Aplikasi tambahan terapi fotodinamik antimikroba pada pengobatan periodontal non-bedah: Tinjauan literatur
- 11 Cara mudah memutihkan gigi palsu
- Drg. Andreas Tjandra dalam
- Drg. Andreas Tjandra dalam
- Clinical performance of a regenerative strategy for intrabony defects: scientific evidence and clinical experience
- Performa klinis strategi regeneratif untuk cacat intra-tulang: bukti sains dan pengalaman klinis
- Performa klinis strategi regeneratif untuk cacat intra-tulang: bukti sains dan pengalaman klinis
- Performa klinis strategi regeneratif untuk cacat intra-tulang: bukti sains dan pengalaman klinis
- Performa klinis strategi regeneratif untuk cacat intra-tulang: bukti saintifik dan pengalaman klinis
- Performa klinis strategi regeneratif untuk kerusakan intra-tulang: bukti saintifik dan pengalaman klinis
- Hello, World!
- Hello, World! I am coming!
- Hello, World! I come
- Good view is scarce
- pursue_it
- Introduction : Strategy for Intrabony defects
- Pendahuluan: Strategi untuk cacat intra-tulang
- Materials & methods: Strategy for intrabony defects
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Bahan & metode: Strategi untuk cacat intra-tulang
- Result: Strategy for intrabony defects
- Hasil: Strategi untuk cacat intra-tulang
- DISCUSSION: strategy for intrabony defects
- PEMBAHASAN: strategi untuk cacat intra-tulang
- PEMBAHASAN: strategi untuk cacat intra-tulang
- PEMBAHASAN: strategi untuk cacat intra-tulang
- Long-Term Tooth Survival Following Regenerative Treatment of Intrabony Defects
- Kelangsungan hidup gigi dalam jangka panjang pasca perawatan regeneratif cacat intra-tulang
- Introduction: Long-term tooth survival
- Pendahuluan: Kelangsungan hidup gigi dalam jangka panjang
- MATERIALS AND METHODS: Long-term tooth survival
- BAHAN DAN METODE: Kelangsungan hidup gigi dalam jangka panjang
- RESULTS: Long-term tooth survival
- HASIL: kelangsungan hidup gigi dalam jangka panjang
- DISCUSSION: Long-term tooth survival
- Pembahasan: Kelangsungan hidup gigi dalam jangka panjang
- Laboratory tests for dentists (1)
- Tes laboratorium untuk dokter gigi
- Laboratory tests for dentists (2)
- Laboratory tests for dentists (3)
- Tes laboratorium bagi dokter gigi (1)
- Tes laboratorium bagi dokter gigi (2)
- Tes laboratorium bagi dokter gigi (3)
- Effect of denture base reinforcement using light cured e-glass fibers on the level of salivary immunoglobulin A
- Pengaruh penguatan dasar gigi tiruan pakai e-serat kaca light-cured pada tingkat imunoglobulin saliva A
- Introduction: Effect of denture base reinforcement
- Pendahuluan: pengaruh penguatan dasar gigi tiruan
- Material & methods: Effect of denture base reinforcement
- Bahan & Metode: Efek penguatan basis gigi tiruan
- Results: Effect of denture base reinforcement
- Hasil: Efek penguatan basis gigi tiruan
- Discussion: Effect of denture base reinforcement
- Uraian: Efek penguatan basis gigi tiruan
- Clinical case: effect of denture base reinforcement
- Berapa harga implant gigi 2020 lengkap dari mula sampai tuntas?
- hello world
- Jaga imunitas : langkah 1 hadapi virus Corona [dsj]
- Table : Partially limiting design
- Table : Partially limiting design
- Table : Partially limiting design
- Post-extraction socket
- Post-extraction socket
- Post-extraction socket
- Kenapa pasien COVID-19 bisa meninggal?
- Anatomical features of the alveolar process
- Anatomical features of the alveolar process
- Anatomical features of the alveolar process
- Jepang lebih dekat Wuhan daripada AS tapi lebih sedikit kasus Corona
- 19-nCOV & COVID-19 : bedanya apa?
- Gejala sakit COVID-19
- Warta baik di tengah pandemi COVID-19
- Golongan wardah bebanten COVID-19 terbanyak
- Siapa yang bisa menularkan COVID-19 dan 19-nCOV?
- Pasien COVID-19 yang pertama diketahui
- Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1
- Apa warna riil virus corona yang sebenarnya?
- Warta Baik: Biofarma produksi RT-PCR untuk 50 ribu test
- Warta baik: peneliti menemukan antibody Covid-19
- FPDB meluncurkan pedoman untuk kembali praktek pasca pandemi COVID-19
- Pasien robot membantu melatih dokter gigi masa datang
- Bakteri dalam mulut & alzheimer
- Klasifikasi risiko paparan SARS-CoV-2 (19-nCoV)
- Jepang membolehkan komersialisasi OCP/Col untuk bedah oral
- Rasa logam kala batuk gejala penyakit
- Arti 10 warna lidah
- 10 Pemicu sakit gigi
- Zirconium
- Sejarah zirconium
- Pilih crown emas atau porselen?
- Pemakai implant gigi hati-hati makan ini
- Biomekanika implant
- Kapasitas implant menanggung beban
- Angulasi dan tatanan
- Finite Element Analysis (FEA)
- Botox di kedokteran gigi
- Membersihkan implant gigi di rumah
- Modifikasi implant berbasis obat
- Periodontist
- Perawatan periodontal non-bedah
- Sikat gigi dulu apa flossing dulu?
- Teh hijau tawar dapat mengokohkan gigi
- Perawatan laser
- Penggunaan sedasi tingkat menengah oleh periodontist
- Prosedur bedah plastik periodontal
- Graft gusi bebas di seputar implant posterior
- undefined. undefined
- Abstract
- Abstract
- CLONE-Abstract : Machine learning approach to drivers of bank lending: evidence from an emerging economy
- undefined
- CLONE-undefined
- undefined
- CLONE-Introduction : Machine learning approach to drivers of bank lending: evidence from an emerging economy [1]
- Introduction : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- Introduction : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- Introduction : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- Introduction : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- Introduction : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- Introduction : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- Introduction : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- Literature review : Machine learning approach to drivers of bank lending: evidence from an emerging economy [1]
- Literature review : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- Literature review : Machine learning approach to drivers of bank lending: evidence from an emerging economy [3]
- Banking sector in Turkey : Machine learning approach to drivers of bank lending: evidence from an emerging economy [1]
- Banking sector in Turkey : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- Datasets : Machine learning approach to drivers of bank lending: evidence from an emerging economy [1]
- Datasets : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- Datasets : Machine learning approach to drivers of bank lending: evidence from an emerging economy [3]
- Datasets : Machine learning approach to drivers of bank lending: evidence from an emerging economy [4]
- Methodology : Machine learning approach to drivers of bank lending: evidence from an emerging economy [1]
- Methodology : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- Methodology : Machine learning approach to drivers of bank lending: evidence from an emerging economy [3]
- Methodology : Machine learning approach to drivers of bank lending: evidence from an emerging economy [4]
- Methodology : Machine learning approach to drivers of bank lending: evidence from an emerging economy [5]
- Methodology : Machine learning approach to drivers of bank lending: evidence from an emerging economy [6]
- Empirical results : Machine learning approach to drivers of bank lending: evidence from an emerging economy [1]
- Empirical results : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- Empirical results : Machine learning approach to drivers of bank lending: evidence from an emerging economy [3]
- Empirical results : Machine learning approach to drivers of bank lending: evidence from an emerging economy [4]
- Empirical results : Machine learning approach to drivers of bank lending: evidence from an emerging economy [5]
- Empirical results : Machine learning approach to drivers of bank lending: evidence from an emerging economy [6]
- Empirical results : Machine learning approach to drivers of bank lending: evidence from an emerging economy [7]
- Empirical results : Machine learning approach to drivers of bank lending: evidence from an emerging economy [8]
- Empirical results : Machine learning approach to drivers of bank lending: evidence from an emerging economy [9]
- Empirical results : Machine learning approach to drivers of bank lending: evidence from an emerging economy [10]
- Empirical results : Machine learning approach to drivers of bank lending: evidence from an emerging economy [11]
- Empirical results : Machine learning approach to drivers of bank lending: evidence from an emerging economy [12]
- Discussion and conclusion : Machine learning approach to drivers of bank lending: evidence from an emerging economy [1]
- Discussion and conclusion : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- Discussion and conclusion : Machine learning approach to drivers of bank lending: evidence from an emerging economy [3]
- Availability of data and materials : Machine learning approach to drivers of bank lending: evidence from an emerging economy
- Notes : Machine learning approach to drivers of bank lending: evidence from an emerging economy
- Abbreviations : Machine learning approach to drivers of bank lending: evidence from an emerging economy
- References : Machine learning approach to drivers of bank lending: evidence from an emerging economy [1]
- References : Machine learning approach to drivers of bank lending: evidence from an emerging economy [2]
- References : Machine learning approach to drivers of bank lending: evidence from an emerging economy [3]
- References : Machine learning approach to drivers of bank lending: evidence from an emerging economy [4]
- References : Machine learning approach to drivers of bank lending: evidence from an emerging economy [5]
- References : Machine learning approach to drivers of bank lending: evidence from an emerging economy [6]
- Acknowledgements : Machine learning approach to drivers of bank lending: evidence from an emerging economy
- Funding : Machine learning approach to drivers of bank lending: evidence from an emerging economy
- Author information : Machine learning approach to drivers of bank lending: evidence from an emerging economy
- Ethics declarations : Machine learning approach to drivers of bank lending: evidence from an emerging economy
- Additional information : Machine learning approach to drivers of bank lending: evidence from an emerging economy
- Supplementary Information : Machine learning approach to drivers of bank lending: evidence from an emerging economy
- Rights and permissions : Machine learning approach to drivers of bank lending: evidence from an emerging economy
- About this article : Machine learning approach to drivers of bank lending: evidence from an emerging economy
- Abstract : Influence of exposing dental implants into the sinus cavity on survival and complications rate: a systematic review [1]
- Abstract : Influence of exposing dental implants into the sinus cavity on survival and complications rate: a systematic review [1]
- Abstract : Influence of exposing dental implants into the sinus cavity on survival and complications rate: a systematic review [1]
- Abstract : Influence of exposing dental implants into the sinus cavity on survival and complications rate: a systematic review [1]
- Abstract : Influence of exposing dental implants into the sinus cavity on survival and complications rate: a systematic review [1]
- Abstract : Influence of exposing dental implants into the sinus cavity on survival and complications rate: a systematic review [1]
- Abstract : Influence of exposing dental implants into the sinus cavity on survival and complications rate: a systematic review [1]
- Abstract : Influence of exposing dental implants into the sinus cavity on survival and complications rate: a systematic review [1]
- Fig. 1. Graphic representation of implants intruding sinus perforating or not the Schneiderian membrane : Influence of exposing dental implant
- Background : Esthetic evaluation of implant-supported single crowns: a comparison of objective and patient-reported outcomes [2]
- Abstract : Effectiveness and compliance of an oscillating-rotating toothbrush in patients with dental implants: a randomized clinical trial
- Abstract : Effectiveness and compliance of an oscillating-rotating toothbrush in patients with dental implants: a randomized clinical trial
- Abstract : Effectiveness and compliance of an oscillating-rotating toothbrush in patients with dental implants: a randomized clinical trial
- Abstract : Effectiveness and compliance of an oscillating-rotating toothbrush in patients with dental implants: a randomized clinical trial
- Abstract : Effectiveness and compliance of an oscillating-rotating toothbrush in patients with dental implants: a randomized clinical trial
- Abstract : Effectiveness and compliance of an oscillating-rotating toothbrush in patients with dental implants: a randomized clinical trial
- Abstract : Effectiveness and compliance of an oscillating-rotating toothbrush in patients with dental implants: a randomized clinical trial
- Abstract : Effectiveness and compliance of an oscillating-rotating toothbrush in patients with dental implants: a randomized clinical trial
- Abstract : Effectiveness and compliance of an oscillating-rotating toothbrush in patients with dental implants: a randomized clinical trial
- Abstract : Effectiveness and compliance of an oscillating-rotating toothbrush in patients with dental implants: a randomized clinical trial
- Materials and methods : Effect of different angulations and collar lengths of conical hybrid implant abutment on screw loosening after dynamic cyclic loading [1]
- Methods : Efficacy of orthodontic mini implants for en masse retraction in the maxilla: a systematic review and meta-analysis [1]
- Table 2 Average thickness by age group : Thickness of the Schneiderian membrane and its correlation with anatomical structures and demographic parameters using CBCT tomography: a retrospective study
- About this article : Clinical outcomes following surgical treatment of peri-implantitis at grafted and non-grafted implant sites: a retrospective analysis
- Materials and methods : Surgical options in oroantral fistula management: a narrative review [1]
- Materials and methods : Surgical options in oroantral fistula management: a narrative review [13]
- Materials and methods : Surgical options in oroantral fistula management: a narrative review [13]
- Results : In vitro surface characteristics and impurity analysis of five different commercially available dental zirconia implants [1]
- Results : In vitro surface characteristics and impurity analysis of five different commercially available dental zirconia implants [1]
- Discussion : Is antral membrane balloon elevation truly minimally invasive technique in sinus floor elevation surgery? A systematic review [1]
- Discussion : Is antral membrane balloon elevation truly minimally invasive technique in sinus floor elevation surgery? A systematic review [1]
- References : Is antral membrane balloon elevation truly minimally invasive technique in sinus floor elevation surgery? A systematic review [2]
- References : Is antral membrane balloon elevation truly minimally invasive technique in sinus floor elevation surgery? A systematic review [2]
- Acknowledgements : Is antral membrane balloon elevation truly minimally invasive technique in sinus floor elevation surgery? A systematic review
- Acknowledgements : Is antral membrane balloon elevation truly minimally invasive technique in sinus floor elevation surgery? A systematic review
- Abstract : Prospective multicenter non-randomized controlled study on intraosseous stability and healing period for dental implants in the posterior region
- Abstract : Prospective multicenter non-randomized controlled study on intraosseous stability and healing period for dental implants in the posterior region
- Abstract : Postgraduate education in dental implantology in the United Kingdom: a review
- Abstract : Postgraduate education in dental implantology in the United Kingdom: a review
- Review : Postgraduate education in dental implantology in the United Kingdom: a review [1]
- Review : Postgraduate education in dental implantology in the United Kingdom: a review [1]
- Review : Postgraduate education in dental implantology in the United Kingdom: a review [2]
- Review : Postgraduate education in dental implantology in the United Kingdom: a review [2]
- Review : Postgraduate education in dental implantology in the United Kingdom: a review [4]
- Review : Postgraduate education in dental implantology in the United Kingdom: a review [4]
- Review : Postgraduate education in dental implantology in the United Kingdom: a review [7]
- Review : Postgraduate education in dental implantology in the United Kingdom: a review [7]
- Conclusion : Postgraduate education in dental implantology in the United Kingdom: a review
- Conclusion : Postgraduate education in dental implantology in the United Kingdom: a review
- References : Postgraduate education in dental implantology in the United Kingdom: a review
- References : Postgraduate education in dental implantology in the United Kingdom: a review
- Results : Diagnostic ability of limited volume cone beam computed tomography with small voxel size in identifying the superior and inferior walls of the mandibular canal
- Results : Diagnostic ability of limited volume cone beam computed tomography with small voxel size in identifying the superior and inferior walls of the mandibular canal
- Ethics declarations : Primary peri-implant oral intra-epithelial neoplasia/carcinoma in situ: a case report considering risk factors for carcinogenesis
- Ethics declarations : Primary peri-implant oral intra-epithelial neoplasia/carcinoma in situ: a case report considering risk factors for carcinogenesis
- Ethics declarations : Novel expandable short dental implants in situations with reduced vertical bone height—technical note and first results
- Ethics declarations : Novel expandable short dental implants in situations with reduced vertical bone height—technical note and first results
- Methods : Correlations between clinical parameters in implant maintenance patients: analysis among healthy and history-of-periodontitis groups [1]
- Methods : Correlations between clinical parameters in implant maintenance patients: analysis among healthy and history-of-periodontitis groups [1]
- Discussion : Comparison of three different methods of internal sinus lifting for elevation heights of 7 mm: an ex vivo study [1]
- Discussion : Comparison of three different methods of internal sinus lifting for elevation heights of 7 mm: an ex vivo study [1]
- Conclusions : Comparison of three different methods of internal sinus lifting for elevation heights of 7 mm: an ex vivo study
- Conclusions : Comparison of three different methods of internal sinus lifting for elevation heights of 7 mm: an ex vivo study
- About this article : Comparison of three different methods of internal sinus lifting for elevation heights of 7 mm: an ex vivo study
- About this article : Comparison of three different methods of internal sinus lifting for elevation heights of 7 mm: an ex vivo study
- Background : Electro-chemical deposition of nano hydroxyapatite-zinc coating on titanium metal substrate [2]
- Background : Electro-chemical deposition of nano hydroxyapatite-zinc coating on titanium metal substrate [2]
- Discussion : A novel non-surgical method for mild peri-implantitis- a multicenter consecutive case series [2]
- Discussion : A novel non-surgical method for mild peri-implantitis- a multicenter consecutive case series [2]
- Conclusions : A novel non-surgical method for mild peri-implantitis- a multicenter consecutive case series
- Conclusions : A novel non-surgical method for mild peri-implantitis- a multicenter consecutive case series
- References : The influence of surface texture and wettability on initial bacterial adhesion on titanium and zirconium oxide dental implants [1]
- References : The influence of surface texture and wettability on initial bacterial adhesion on titanium and zirconium oxide dental implants [1]
- Table 1 Arithmetic average of surface roughness R
- Table 1 Arithmetic average of surface roughness R
- Erratum : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Erratum : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Reference : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Reference : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Author information : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Author information : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Additional information : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Additional information : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- About this article : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- About this article : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Background : The effect of membrane exposure on lateral ridge augmentation: a case-controlled study [2]
- Background : The effect of membrane exposure on lateral ridge augmentation: a case-controlled study [2]
- Abstract : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Abstract : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Background : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [1]
- Background : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [1]
- Background : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [2]
- Background : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [2]
- Methods : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [1]
- Methods : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [1]
- Methods : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [3]
- Methods : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [3]
- Results : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Results : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Discussion : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [2]
- Discussion : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [2]
- Conclusions : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Conclusions : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- References : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [1]
- References : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [1]
- References : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [2]
- References : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [2]
- Acknowledgements : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Acknowledgements : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Author information : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Author information : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Rights and permissions : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Rights and permissions : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Abstract : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Abstract : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Background : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Background : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Methods : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [1]
- Methods : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [2]
- Methods : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [2]
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [1]
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [1]
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [2]
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [2]
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [3]
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [3]
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [4]
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [4]
- Conclusions : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Conclusions : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- References : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [1]
- References : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [1]
- References : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [2]
- References : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [2]
- References : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [3]
- References : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [3]
- References : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [4]
- References : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [4]
- Acknowledgements : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Acknowledgements : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Author information : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Author information : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Rights and permissions : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Rights and permissions : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- About this article : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- About this article : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Table 3 Surface areas changes of access-hole filling. Unit: % : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Table 3 Surface areas changes of access-hole filling. Unit: % : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- About this article : Osseointegration of standard and mini dental implants: a histomorphometric comparison
- About this article : Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Material and methods : Alveolar ridge preservation with autologous particulated dentin—a case series [1]
- Material and methods : Alveolar ridge preservation with autologous particulated dentin—a case series [1]
- Material and methods : Alveolar ridge preservation with autologous particulated dentin—a case series [1]
- References : Treatment with teriparatide for advanced bisphosphonate-related osteonecrosis of the jaw around dental implants: a case report [3]
- References : Treatment with teriparatide for advanced bisphosphonate-related osteonecrosis of the jaw around dental implants: a case report [3]
- Methods : Evaluation of effectiveness of concentrated growth factor on osseointegration [1]
- Methods : Evaluation of effectiveness of concentrated growth factor on osseointegration [1]
- Discussion : Customized SmartPeg for measurement of resonance frequency of mini dental implants [3]
- Discussion : Customized SmartPeg for measurement of resonance frequency of mini dental implants [3]
- References : Customized SmartPeg for measurement of resonance frequency of mini dental implants [1]
- References : Customized SmartPeg for measurement of resonance frequency of mini dental implants [1]
- Background : Case report on managing incomplete bone formation after bilateral sinus augmentation using a palatal approach and a dilating balloon technique [2]
- Background : Case report on managing incomplete bone formation after bilateral sinus augmentation using a palatal approach and a dilating balloon technique [2]
- Conclusions : Case report on managing incomplete bone formation after bilateral sinus augmentation using a palatal approach and a dilating balloon technique
- Conclusions : Case report on managing incomplete bone formation after bilateral sinus augmentation using a palatal approach and a dilating balloon technique
- Acknowledgements : Case report on managing incomplete bone formation after bilateral sinus augmentation using a palatal approach and a dilating balloon technique
- Acknowledgements : Case report on managing incomplete bone formation after bilateral sinus augmentation using a palatal approach and a dilating balloon technique
- Author information : Case report on managing incomplete bone formation after bilateral sinus augmentation using a palatal approach and a dilating balloon technique
- Author information : Case report on managing incomplete bone formation after bilateral sinus augmentation using a palatal approach and a dilating balloon technique
- Rights and permissions : Case report on managing incomplete bone formation after bilateral sinus augmentation using a palatal approach and a dilating balloon technique
- Rights and permissions : Case report on managing incomplete bone formation after bilateral sinus augmentation using a palatal approach and a dilating balloon technique
- About this article : Case report on managing incomplete bone formation after bilateral sinus augmentation using a palatal approach and a dilating balloon technique
- About this article : Case report on managing incomplete bone formation after bilateral sinus augmentation using a palatal approach and a dilating balloon technique
- Background : Relation between the stability of dental implants and two biological markers during the healing period: a prospective clinical study [1]
- Background : Relation between the stability of dental implants and two biological markers during the healing period: a prospective clinical study [1]
- Discussion : Mucositis, peri-implantitis, and survival and success rates of oxide-coated implants in patients treated for periodontitis 3- to 6-year results of a case-series study [1]
- Discussion : Mucositis, peri-implantitis, and survival and success rates of oxide-coated implants in patients treated for periodontitis 3- to 6-year results of a case-series study [1]
- Discussion : Mucositis, peri-implantitis, and survival and success rates of oxide-coated implants in patients treated for periodontitis 3- to 6-year results of a case-series study [2]
- Discussion : Mucositis, peri-implantitis, and survival and success rates of oxide-coated implants in patients treated for periodontitis 3- to 6-year results of a case-series study [2]
- Author information : Primary peri-implant oral intra-epithelial neoplasia/carcinoma in situ: a case report considering risk factors for carcinogenesis [1]
- Author information : Primary peri-implant oral intra-epithelial neoplasia/carcinoma in situ: a case report considering risk factors for carcinogenesis [1]
- Author information : Primary peri-implant oral intra-epithelial neoplasia/carcinoma in situ: a case report considering risk factors for carcinogenesis [2]
- Author information : Primary peri-implant oral intra-epithelial neoplasia/carcinoma in situ: a case report considering risk factors for carcinogenesis [2]
- Table 1 Arithmetic average of surface roughness R
- Table 1 Arithmetic average of surface roughness R
- Erratum : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Additional information : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Additional information : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Rights and permissions : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Rights and permissions : Erratum to: Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Methods : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [2]
- Methods : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [2]
- Discussion : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [2]
- Discussion : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles [2]
- Conclusions : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Conclusions : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [1]
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [1]
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [2]
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [2]
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [4]
- Discussion : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [4]
- Conclusions : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Conclusions : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- References : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [3]
- References : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [3]
- References : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [4]
- References : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study [4]
- Acknowledgements : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Acknowledgements : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Author information : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Author information : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Rights and permissions : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Rights and permissions : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- About this article : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- About this article : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Abstract : Cellular fluid shear stress on implant surfaces—establishment of a novel experimental set up
- Abstract : Cellular fluid shear stress on implant surfaces—establishment of a novel experimental set up
- Background : Cellular fluid shear stress on implant surfaces—establishment of a novel experimental set up [1]
- Background : Cellular fluid shear stress on implant surfaces—establishment of a novel experimental set up [1]
- Abstract : Cellular fluid shear stress on implant surfaces—establishment of a novel experimental set up
- Abstract : Cellular fluid shear stress on implant surfaces—establishment of a novel experimental set up
- Abstract : Cellular fluid shear stress on implant surfaces—establishment of a novel experimental set up
- Abstract : Cellular fluid shear stress on implant surfaces—establishment of a novel experimental set up
- Background : Cellular fluid shear stress on implant surfaces—establishment of a novel experimental set up [1]
- Background : Cellular fluid shear stress on implant surfaces—establishment of a novel experimental set up [1]
- Background : Cellular fluid shear stress on implant surfaces—establishment of a novel experimental set up [2]
- Background : Cellular fluid shear stress on implant surfaces—establishment of a novel experimental set up [2]
- Abstract : Cellular fluid shear stress on implant surfaces—establishment of a novel experimental set up
- Abstract : Osteogenesis ability of CAD/CAM porous zirconia scaffolds enriched with nano-hydroxyapatite particles
- Abstract : Sandwich bone graft for vertical augmentation of the posterior maxillary region: a case report with 9-year follow-up
- Abstract : Comparison of access-hole filling materials for screw retained implant prostheses: 12-month in vivo study
- Abstract : Comparative evaluation of the stability of two different dental implant designs and surgical protocols—a pilot study [1]
- Abstract : Osseointegration of standard and mini dental implants: a histomorphometric comparison
- Abstract : Segmental sandwich osteotomy and tunnel technique for three-dimensional reconstruction of the jaw atrophy: a case report [1]
- Abstract : Evaluation of symptomatic maxillary sinus pathologies using panoramic radiography and cone beam computed tomography—influence of professional training
- Abstract : Alveolar ridge preservation with autologous particulated dentin—a case series
- Abstract : Treatment with teriparatide for advanced bisphosphonate-related osteonecrosis of the jaw around dental implants: a case report
- Abstract : Impact of maxillary sinus augmentation on oral health-related quality of life
- Abstract : A novel report on the use of an oncology zygomatic implant-retained maxillary obturator in a paediatric patient
- Abstract : Short-term follow-up of masticatory adaptation after rehabilitation with an immediately loaded implant-supported prosthesis: a pilot assessment
- Abstract : Evaluation of effectiveness of concentrated growth factor on osseointegration
- Abstract : Platelet-rich fibrin prepared from stored whole-blood samples
- Abstract : Zirconia implants and peek restorations for the replacement of upper molars
- Abstract : Customized SmartPeg for measurement of resonance frequency of mini dental implants [1]
- Abstract : Case report on managing incomplete bone formation after bilateral sinus augmentation using a palatal approach and a dilating balloon technique
- Abstract : Maxillary segmental osteoperiosteal flap with simultaneous placement of dental implants: case report of a novel technique
- Abstract : Dental implants and grafting success remain high despite large variations in maxillary sinus mucosal thickening
- Abstract : Relation between the stability of dental implants and two biological markers during the healing period: a prospective clinical study
- Abstract : “Reverse torque of 30 Ncm applied to dental implants as test for osseointegration”—a human observational study
- Abstract : Relation between the stability of dental implants and two biological markers during the healing period: a prospective clinical study
- Abstract : “Reverse torque of 30 Ncm applied to dental implants as test for osseointegration”—a human observational study
- Fig. 2. Informed consent for patients : “Reverse torque of 30 Ncm applied to dental implant
- Fig. 2. Kaplan-Meier implant survival curves for augmentation procedures : Retrospective analysis of 10,000 implant
- Fig. 2. Kaplan-Meier implant survival curves for augmentation procedures : Retrospective analysis of 10,000 implant
- Fig. 2. Kaplan-Meier implant survival curves for augmentation procedures : Retrospective analysis of 10,000 implant
- Fig. 2. Kaplan-Meier implant survival curves for augmentation procedures : Retrospective analysis of 10,000 implant
- Fig. 2. Kaplan-Meier implant survival curves for augmentation procedures : Retrospective analysis of 10,000 implant
- Fig. 2. Kaplan-Meier implant survival curves for augmentation procedures : Retrospective analysis of 10,000 implant
- Fig. 2. Kaplan-Meier implant survival curves for augmentation procedures : Retrospective analysis of 10,000 implant
- Abstract : Vitamin D deficiency in early implant failure: two case reports
- Abstract : Twist removal of healed vs. nonhealed implants—a mechanical and histological study in mini pigs
- Abstract : To what extent residual alveolar ridge can be preserved by implant? A systematic review
- Abstract : A prospective study of the relationship between patient character and blood pressure in dental implant surgery
- Abstract : Prospective cohort study of dental implant success rate in patients with AIDS
- Abstract : Osseointegration of TI6Al4V dental implants modified by thermal oxidation in osteoporotic rabbits
- Abstract : Biomechanical effects of offset placement of dental implants in the edentulous posterior mandible [1]
- Abstract : Continuous intra-sinus bone regeneration after nongrafted sinus lift with a PLLA mesh plate device and dental implant placement in an atrophic posterior maxilla: a case report
- Abstract : Continuous intra-sinus bone regeneration after nongrafted sinus lift with a PLLA mesh plate device and dental implant placement in an atrophic posterior maxilla: a case report
- Abstract : Continuous intra-sinus bone regeneration after nongrafted sinus lift with a PLLA mesh plate device and dental implant placement in an atrophic posterior maxilla: a case report
- Abstract : Continuous intra-sinus bone regeneration after nongrafted sinus lift with a PLLA mesh plate device and dental implant placement in an atrophic posterior maxilla: a case report
- Abstract : Continuous intra-sinus bone regeneration after nongrafted sinus lift with a PLLA mesh plate device and dental implant placement in an atrophic posterior maxilla: a case report
- Abstract : Continuous intra-sinus bone regeneration after nongrafted sinus lift with a PLLA mesh plate device and dental implant placement in an atrophic posterior maxilla: a case report
- Background : Continuous intra-sinus bone regeneration after nongrafted sinus lift with a PLLA mesh plate device and dental implant placement in an atrophic posterior maxilla: a case report
- Case presentation : Continuous intra-sinus bone regeneration after nongrafted sinus lift with a PLLA mesh plate device and dental implant placement in an atrophic posterior maxilla: a case report [1]
- Abstract : Continuous intra-sinus bone regeneration after nongrafted sinus lift with a PLLA mesh plate device and dental implant placement in an atrophic posterior maxilla: a case report
- Table 1
- Table 2
- Table 3
- Table 3 Three-way ANOVA (displacement in the buccolingual direction [
- Table 3 Three-way ANOVA (displacement in the buccolingual direction [x
- Table 4
- Table 4 Three-way ANOVA (displacement in the mesiodistal direction [y
- Table 4 Three-way ANOVA (displacement in the mesiodistal direction [
- Table 5 Three-way ANOVA (displacement in the inferior-superior direction [
- Table 6
- Table 7
- Table 1
- Table 2
- Table 3
- Table 3 Bacterial and fungal analysis: peri-implantitis sites (n
- Table 3 Bacterial and fungal analysis: peri-implantitis sites (
- Table 4
- Table 4 Bacterial and fungal analysis: healthy implant sites (n
- Table 4 Bacterial and fungal analysis: healthy implant sites (n = 10 patients)
- Table 5
- Table 5 Bacterial and fungal analysis: tooth sites (
- Table 5 Bacterial and fungal analysis: tooth sites (n = 10 patients)
- Table 1
- Table 2
- Table 3
- Table 1
- Table 2
- Table 3
- Table 3 Summary of findings from the included studies (
- Table 3 Summary of findings from the included studies (n
- Table 4 Summary of biological processes and associated genes reported in the included studies
- Table 1
- Table 2
- Table 3
- Table 4
- Table 1
- Table 2
- Table 3
- Highlights : Is maxillary diastema an appropriate site for implantation in rats?
- Availability of data and materials : Viability and collagen secretion by fibroblasts on titanium surfaces with different acid-etching protocols
- Availability of data and materials : Viability and collagen secretion by fibroblasts on titanium surfaces with different acid-etching protocols
- Availability of data and materials : Viability and collagen secretion by fibroblasts on titanium surfaces with different acid-etching protocols
- Availability of data and materials : Viability and collagen secretion by fibroblasts on titanium surfaces with different acid-etching protocols
- Availability of data and materials : Viability and collagen secretion by fibroblasts on titanium surfaces with different acid-etching protocols
- References : Viability and collagen secretion by fibroblasts on titanium surfaces with different acid-etching protocols [1]
- References : Viability and collagen secretion by fibroblasts on titanium surfaces with different acid-etching protocols [2]
- References : Viability and collagen secretion by fibroblasts on titanium surfaces with different acid-etching protocols [3]
- Acknowledgements : Viability and collagen secretion by fibroblasts on titanium surfaces with different acid-etching protocols
- Acknowledgements : Viability and collagen secretion by fibroblasts on titanium surfaces with different acid-etching protocols
- Fig. 1. Scanning electron microscopy and laser interferometry. a, d Machined surface. b, e 20-min
- Fig. 1. Scanning electron microscopy and laser interferometry. a, d Machined surface. b, e 20-min
- Background : Vestibular bone thickness of the mandible in relation to the mandibular canal—a retrospective CBCT-based study [1]
- Background : Vestibular bone thickness of the mandible in relation to the mandibular canal—a retrospective CBCT-based study [1]
- Background : Vestibular bone thickness of the mandible in relation to the mandibular canal—a retrospective CBCT-based study [1]
- undefined : Patients’ appreciation of pre-implant
- Table 5 Patient reported outcomes of bone graft harvesting surgery per group : [1]
- Table 5 Patient reported outcomes of bone graft harvesting surgery per group : [1]
- Table 5 Patient reported outcomes of bone graft harvesting surgery per group : [1]
- Table 5 Patient reported outcomes of bone graft harvesting surgery per group : [1]
- Table 5 Patient reported outcomes of bone graft harvesting surgery per group : [1]
- Table 5 Patient reported outcomes of bone graft harvesting surgery per group : [1]
- Table 5 Patient reported outcomes of bone graft harvesting surgery per group : [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Abstract : Patients’ appreciation of pre-implant augmentation of the severely resorbed maxilla with calvarial or anterior iliac crest bone:a randomized controlled trial [1]
- Fig. 2 - Significant difference between groups in mean post-operative
- Fig. 2 - Significant difference between groups in mean post-operative
- Fig. 2 - Significant difference between groups in mean post-operative
- Fig. 2 - Significant difference between groups in mean post-operative
- Fig. 2 - Significant difference between groups in mean post-operative
- Fig. 2 - Significant difference between groups in mean post-operative
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Post Title
- Pendanaan : Kasus langka osteonekrosis rahang terkait bevacizumab terkait dengan implan gigi
- Pendanaan : Kasus langka osteonekrosis rahang terkait bevacizumab terkait dengan implan gigi
- Pendanaan : Kasus langka osteonekrosis rahang terkait bevacizumab terkait dengan implan gigi
- Pendanaan : Kasus langka osteonekrosis rahang terkait bevacizumab terkait dengan implan gigi
- Pendanaan : Kasus langka osteonekrosis rahang terkait bevacizumab terkait dengan implan gigi
- Discussion : Kasus langka osteonekrosis rahang terkait bevacizumab terkait dengan implan gigi [2]
- Discussion : Kasus langka osteonekrosis rahang terkait bevacizumab terkait dengan implan gigi [2]
- Kesimpulan : Kasus langka osteonekrosis rahang terkait bevacizumab terkait dengan implan gigi
- Abbreviations : Kasus langka osteonekrosis rahang terkait bevacizumab terkait dengan implan gigi
- Abbreviations : Kasus langka osteonekrosis rahang terkait bevacizumab terkait dengan implan gigi
- Abbreviations : Kasus langka osteonekrosis rahang terkait bevacizumab terkait dengan implan gigi
- Referensi : Kasus langka osteonekrosis rahang terkait bevacizumab terkait dengan implan gigi [3]
- Informasi tambahan : Kasus langka osteonekrosis rahang terkait bevacizumab terkait dengan implan gigi
- Latar Belakang : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [1]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]methods_ketebalan_tulang_vestibular_mandibula_dalam_kaitannya_dengan_kanal_mandibulastudi_berbasis_cbct_retrospektif_2_5hXwY
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]metho
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]method
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]methods_ketebalan_tulang_vestibular_mandibula_dalam_kaitannya_dengan_kanal_mandibulastudi_berbasis_cbct_retrospektif_2_dKW8N
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]methods_ketebalan_tulang_vestibular_mandibula_dalam_kaitannya_dengan_kanal_mandibulastudi_berbasis_cbct_retrospektif_2_uAywQ
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT ret
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibulastudi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya de
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]
- Methods : Ketebalan tulang vestibular mandibula dalam kaitannya dengan kanal mandibula—studi berbasis CBCT retrospektif [2]